Diagnosis of Systemic Lupus Erythematosus
Systemic Lupus Erythematosus (SLE or Lupus) is a difficult disease to diagnose. Because the signs/symptoms can occur in a wide variety of organ systems, it is difficult to pinpoint the diagnosis of SLE initially. The diagnosis of SLE is based on clinical evaluation and laboratory evidence.
The American College of Rheumatology (ACR) has developed specific criteria to aid in the diagnosis of SLE. The SLICC (Systemic Lupus International Collaborating Clinics) group in collaboration with the ACR recommendations have stated a person is diagnosed with SLE if they have biopsy proven lupus nephritis with ANA or anti-dsDNA antibodies positive laboratories; or if at least 4 of the 11 ACR criteria have been met including at least 1 clinical and 1 immunologic.
The American College of Rheumatology (ACR) has developed a mnemonic to help in identifying the diagnostic criteria. The mnemonic is SOAP BRAIN MD. If the patient meets at least 4 of those ACR criteria, then a clinical diagnosis of SLE may be made.
- S stands for serositis.
- O stands for oral ulcers.
- A stands for arthritis.
- P stands for photosensitivity.
- B stands for blood disorders.
- R stands for renal involvement.
- A stands for ANA (antinuclear antibodies).
- I stand for immunologic laboratory tests (dsDNA, anti-smith ab).
- N stands for neurologic disorders.
- M stands for malar rash (which is the butterfly rash on the face, cheek and nose bridge).
- D stands for a discoid rash.
Laboratory testing can be beneficial in SLE diagnosis. Routine blood work including CBC, ESR, CMP, UA and ANA can be very beneficial.
The CBC is a complete blood count. It evaluates the patient’s red blood cells, white blood cells, platelets and haemoglobin. Patients with SLE may develop decreased levels of their white blood cells and their platelets, and so if there are abnormalities in these areas it can be an indicator to look further. Patients with SLE also develop hemolytic anaemia in many cases, so evaluating the haemoglobin can be beneficial.
The Erythrocyte Sedimentation Rate (ESR) may be elevated in inflammatory conditions as well as in Lupus, so it can be an appropriate indicator that there is a systemic process occurring but it is not specific for Lupus.
Evaluating the CMP allows for evaluation of the kidney and liver functions. If SLE is attacking the kidneys and/or the liver there is likely to be damage to those organs, which can show up in the lab values.
A urinalysis (UA) is important because it allows for the urine to be analyzed for protein or red blood cells; both of which can be present in patients who have SLE.
The ANA (antinuclear antibody) is often positive in patients with Lupus. However, it is not a very specific test; thus, there are patients who have a positive ANA that does not have SLE. If SLE is suspected, more specific antibody testing may be suggested.
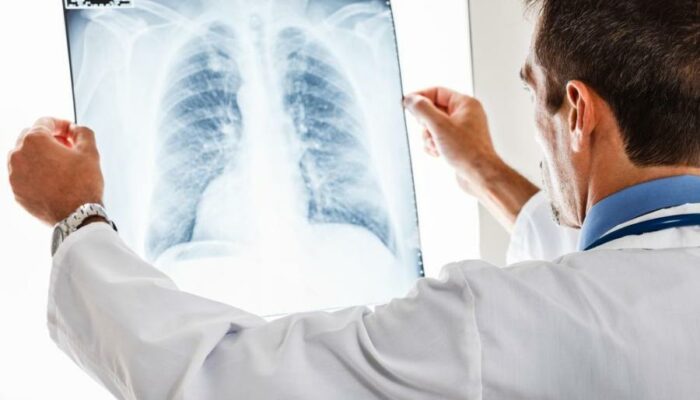
Imaging tests also play a key role in diagnosing Systemic Lupus Erythematosus (SLE or Lupus). If the lungs or heart are being attacked by the immune system in SLE, then a chest X-ray and echocardiogram may be useful. The chest X-ray is a good way to evaluate the lungs for fluid and/or inflammation. The echocardiogram is used to evaluate the values and ejection fraction of the heart. Other imaging studies to evaluate the affected organ systems may be appropriate to help diagnose SLE.
One of the criteria SLICC has for SLE diagnosis is biopsy-proven renal nephritis. SLE commonly attacks the kidneys. Therefore, a biopsy of the kidneys can provide a conclusive diagnosis of SLE nephritis.