Risks Associated With Blood Transfusion
Blood Transfusion Risks And Complications
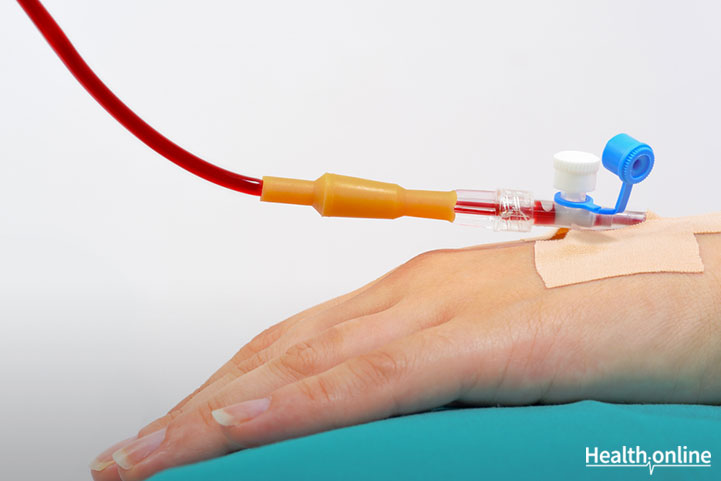
There are minor risks related to blood collection. The materials used for each donation are new, sterile, and disposable so there is virtually no risk of blood-borne infection.
Since only a pint of blood is collected per donation, the donor can continue with normal daily activities after recovering for a few minutes. The body replenishes the plasma after 24 hours and red blood cells are replaced in approximately 6 weeks.
Some experience minor temporary bruising at the collection site. In rare cases, phlebitis—inflammation of the vein—may occur. Swelling can be reduced by applying ice for 10-15minutes on the first day and then a warm compress to the area multiple times a day. A multicolored bruise may be visible for up to 10 days. Those with clotting problems may also experience continuous bleeding. Drink lots of liquids and get plenty of rest.
Blood Transfusion Risks
Mild side effects
In most cases, transfusion has little to no side effects. These side effects include headaches, itchiness, difficulty breathing, a rash or a fever. Any side effects experienced can be easily treated with medication. In some cases, more severe side effects may be experienced such as extreme difficulty breathing, chest pains, and low blood pressure.
Allergic Reactions
Despite using compatible blood for donations, blood donation recipients may experience an allergic reaction to the blood. Some signs of such a reaction include feelings of anxiety, chest pain, back pain, difficulty breathing, sweating, feeling cold, feeling warm, a rapid decrease in blood pressure, a quick increase in heart rate, or nausea. Once an allergic reaction is observed, the health care provider assisting with the blood transfusion will stop the transfusion and assess the patient’s response. If the response is relatively mild, the transfusion will continue.
Transfusion Reaction
During a blood transfusion, it is vital that blood with the compatible antigens are transfused into the recipient. When incompatible blood is transfused, the recipient will experience transfusion reaction. Transfusion reaction is when the antibodies in the recipient’s plasma attack and destroy donor blood. The effects of a transfusion reaction can range from mild to deadly.
Acute Immune Hemolytic Reaction
Along the lines of a transfusion reaction is an acute immune hemolytic reaction. This is a strong reaction following a donation with either incompatible blood or blood that the body does not accept. The recipient’s immune system attacks donated red blood cells. These attacked cells then produce and release harmful elements that can damage the kidneys. Patients undergoing this reaction experience feeling of extreme cold or hot, nausea, back pains, chest pains and dark urine. Like with an allergic reaction, the transfusion will be stopped immediately when a sign of acute immune hemolytic reaction is observed.
Delayed Hemolytic Reaction
A delayed hemolytic reaction is a gradual attack on red blood cells. The symptoms are much less obvious and may not be noticed until red blood cell levels reach a dangerously low level. Patients that have had blood transfusions previously are at risk of experiencing these hemolytic reactions.
Transfusion-transmissible Infections
The likelihood of contracting a blood borne infection from a blood transfusion is low. This is especially true in high-income countries. The World Health Organization recommends that donated blood is tested for common, lethal diseases including HIV, Hepatitis B, hepatitis C and syphilis. The prevalence of HIV , hepatitis B, hepatitis C and syphilis is 0.003%, 0.03%, 0.02% and 0.05%, respectively from donations made in high-income countries.
The likelihood of infection inversely increases with the income of the country. Unfortunately, 13 countries cannot screen their donations for at least one of these diseases due to changes in the availability of testing kits. However, even in low-income countries, the likelihood of infection is relatively low. HIV , hepatitis B virus, hepatitis C virus and syphilis infections only occur in 1.08%, 3.7%, 1.03% and 0.9% of transfusions in low-income countries.
Fever
In the days immediately after the blood transfusion, the recipient may experience a slight fever due to an increase in white blood cells from the donation. However, this can be easily treated with medication.
Iron Accumulation
Receiving multiple blood transfusions can result in an accumulation of iron in the patient’s blood. Patients with disease that require multiple transfusions, such as thalassemia or aplastic anemia are especially at risk for this side effect. Accumulation of iron can be harmful as iron can cause damage to multiple vital organs such as the liver and the heart. Patients at risk of iron overload often take iron chelators following the blood transfusion. Iron chelators or chelation therapy involves chelators, or organic compounds that bind to metals. Chelators bind to iron to create a neutral compound that can be excreted.
Lung Injury
Though rare, some patients experience temporary difficulty breathing a few hours after a blood transfusion. This difficulty often subsides shortly. However, in a small minority this difficulty is indicative of a lung injury. Between 5% and 25% of patients with these injuries, primarily patients that were very ill prior to the blood transfer, die do to complications related to the injury. How blood transfusions cause lung injury is not well-understood. Some researchers believe that plasma in donated blood from women that had previously been pregnant contains antibodies that may interfere with lung function. Until the cause is resolved, many hospitals are trying to avoid this reaction by utilizing plasma from women in other ways.




